Acute visual loss as the initial presentation in a child with systemic Burkitt lymphoma
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2013; 34(02): 99-100
DOI: DOI: 10.4103/0971-5851.116188
Abstract
Non-Hodgkin lymphoma (NHL) accounts for 10% of pediatric malignancies and is the third most common malignancy in childhood. We report a previous healthy 3-year-old boy with stage IV Burkitt lymphoma presenting with acute visual loss. In funduscopy his pupils were fixed at 6 mm in diameter without light perception. He started therapy according to the UKCCSG 9003 protocol. The boy didn′t show any visual improvement but some slight light perception despite his partial remission after CYVE II. He died of neutropenic septicemia before his scheduled radiotherapy. In conclusion, loss of vision is a rare presenting sign in NHL. Differential diagnosis is crucial as early diagnosis and effective treatment are important for survival as well as for visual restoration.
Publication History
Article published online:
20 July 2021
© 2013. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Non-Hodgkin lymphoma (NHL) accounts for 10% of pediatric malignancies and is the third most common malignancy in childhood. We report a previous healthy 3-year-old boy with stage IV Burkitt lymphoma presenting with acute visual loss. In funduscopy his pupils were fixed at 6 mm in diameter without light perception. He started therapy according to the UKCCSG 9003 protocol. The boy didn’t show any visual improvement but some slight light perception despite his partial remission after CYVE II. He died of neutropenic septicemia before his scheduled radiotherapy. In conclusion, loss of vision is a rare presenting sign in NHL. Differential diagnosis is crucial as early diagnosis and effective treatment are important for survival as well as for visual restoration.
INTRODUCTION
Non-Hodgkin lymphoma (NHL) accounts for 10% of pediatric malignancies and is the third most common malignancy in childhood. Central nervous system (CNS) involvement in NHL is uncommon occurring in about 10% of cases.[1] Ocular involvement in NHL occurs as primary ocular, central nervous system lymphoma or isolated intraocular lymphoma, but optic nerve and chiasmal disease is very rare. At the time of presentation, signs and symptoms depend on the site and degree of involvement, the stage of the malignancy and the histological subtype of the disease. Although the head and neck region is a common site for extranodal involvement, acute loss of vision is a rare presenting symptom of NHL and only 9 cases are reported.[2]
CASE REPORT
We report a case of a 3-year-old boy with acute visual loss in both eyes, who had been diagnosed with stage IV NHL with bone marrow, abdominal and CNS involvement. The child was admitted with complaint of acute blindness in both eyes without a remarkable past medical history. In funduscopy, his pupils were fixed at 6 mm in diameter without light perception. Cranial magnetic resonance imaging (MRI) demonstrated masses arising within the sphenoid sinus and invading the orbits and ethmoidal sinuses causing bilateral compression on optic nerves [Figure 1] The diagnosis of B-NHL was defined cytologically and immunologically in the bone marrow aspirates and cerebrospinal fluid (CSF). Abdominal computed tomography also depicted tumoral infiltration of the kidneys and abdominal lymphadenopathy. His acute blindness was attributed to optic nerve compression in addition to the high proliferation rate characteristic to Burkitt lymphoma. Once the diagnosis was established, he started therapy according to the UKCCSG 9003 protocol. Response to chemotherapy was monitored by appropriate restaging investigations after COP and CYVE II. The boy did not show any visual improvement but some slight light perception despite his partial remission after CYVE II as depicted in restaging investigations. Unfortunately, he relapsed in the CNS and died secondary to neutropenic septicemia 6 months after diagnosis before his scheduled radiotherapy without ever achieving complete remission.
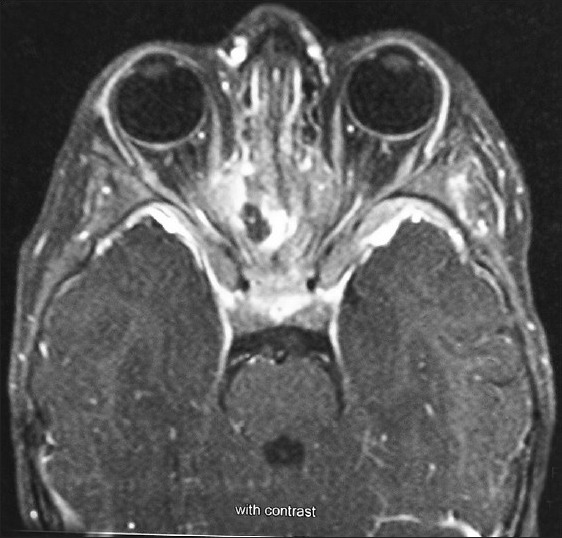
| Fig. 1 Cranial magnetic resonance imaging (MRI) demonstrating masses arising within the sphenoid sinus and invading the orbits and ethmoidal sinuses causing bilateral compression on optic nerves
DISCUSSION
This report describes a patient with systemic Burkitt lymphoma illustrating an important point that loss of vision may be the presenting symptom in systemic NHL at diagnosis. Previous reports have documented optic neuropathy with CNS involvement in adult patients with systemic lymphoma in clinical remission.[3] Although series of pediatric ocular and orbital lymphomas have been reported, optic nerve infiltration from systemic NHL in the pediatric age group at diagnosis are extremely limited.[4] Optic nerve involvement has been associated with lymphomatous infiltration, infections, vincristine-related neuropathy, neurotoxic drugs, radionecrosis and paraneoplasia.[5] Nasal–paranasal oropharyngeal lymphoma affects elderly individuals most commonly. However, it can also occur in children, with a median age of 5 years. In their majority, primary tumors of the paranasal sinuses present with pain and cranial nerve palsies.[6] The diagnosis of paranasal lymphoma involving the optic nerves should also be included in the differential diagnosis of sudden visual loss. Of the nine previous cases already reported, seven children had bilateral blindness and their visual ability improved in only two cases. Mean age of the reported cases was 8.1 years (range 4-16 years old) with our patient being the youngest.
Differential diagnosis is essential since early diagnosis and appropriate treatment are important factors for survival. Optic nerve involvement by systemic lymphoma is thought to occur from direct invasion by tumor cells, which tend to infiltrate cranial and spinal nerves or it may develop as a complication of leptomeningeal lymphomatosis or orbital lymphoma.[7] Although, CNS involvement in NHL is regarded as a bad prognostic factor by using high-dose methotrexate and intrathecal chemotherapy, event-free survival rates have significantly increased up to 75%.[8,9] Radiotherapy even for CNS involvement is probably no further beneficial in addition to chemotherapy. Nevertheless, it is an option usually confined to exceptional circumstances like persistent disease after chemotherapy, like ours.
In conclusion, acute blindness is an extremely rare presenting sign in NHL in children. Neuroimaging is a helpful tool in establishing the diagnosis. Early recognition and prompt management is essential to preserve or maximize visual function.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
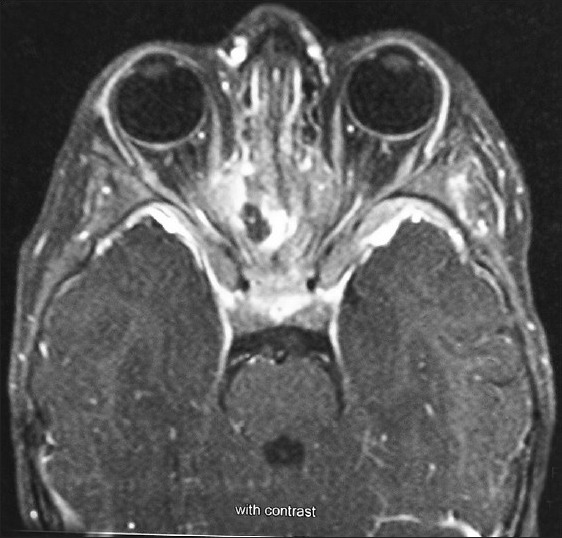
| Fig. 1 Cranial magnetic resonance imaging (MRI) demonstrating masses arising within the sphenoid sinus and invading the orbits and ethmoidal sinuses causing bilateral compression on optic nerves


 PDF
PDF  Views
Views  Share
Share

