A report of the frequency of colorectal carcinoma and involved lymph nodes in South-West Iran
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2016; 37(01): 38-41
DOI: DOI: 10.4103/0971-5851.177014
Abstract
Context: The colorectal cancer (CRC) is the most common malignancy between men and women. CRC has considerable morbidity and mortality, with more than 1000,000 new cases and 500,000 annual deaths. Regional lymph nodes are most common sites of metastasis from colon cancer. Lymph node involvement is an essential factor in enabling the accurate evaluation of prognosis in CRC patients. Aims: In this study, we focused on the frequency of CRC and involved lymph nodes and adequacy of lymph node dissection in patients who referred to the Oncology and Radiotherapy Department of Golestan Hospital in Ahvaz City located in South-West Iran. Setting and Design: We conducted a retrospective study among patients receiving surgical treatment for CRC in the Department of Oncology and Radiotherapy of Golestan Hospital in Ahvaz City located in South-West Iran between 2001 and 2010. Methods and Materials: All patients who underwent resection for CRC by open or laparoscopic approaches were included in the study. Data were collected from patients′ medical records. Statistical Analysis Used: Statistical data were analyzed using SPSS 21. Results: A total of 585 cases with CRC aged from16 to 89 years with mean age of 53-year-old were studied. Average number of dissected nodes was 8 lymph nodes, and lymph nodes were not found in pathology specimen of 61 cases (10.4%). In 199 patients (34.01%), number of dissected lymph nodes was 12 or more and in 386 patients (65.98%), number of dissected lymph nodes was < 12. Conclusion: This study revealed a large amount of patients that had been under over treatment with radiotherapy and the following inability. Lack of removal of sufficient tissue by the surgeon during surgery or an inadequate sample check by a pathologist might lead to an inability to correct staging of the disease as well as the inability to determine the treatment program of the patients and over treatment with radiotherapy and chemotherapy.
Publication History
Article published online:
12 July 2021
© 2016. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Context:
The colorectal cancer (CRC) is the most common malignancy between men and women. CRC has considerable morbidity and mortality, with more than 1000,000 new cases and 500,000 annual deaths. Regional lymph nodes are most common sites of metastasis from colon cancer. Lymph node involvement is an essential factor in enabling the accurate evaluation of prognosis in CRC patients.
Aims:
In this study, we focused on the frequency of CRC and involved lymph nodes and adequacy of lymph node dissection in patients who referred to the Oncology and Radiotherapy Department of Golestan Hospital in Ahvaz City located in South-West Iran.
Setting and Design:
We conducted a retrospective study among patients receiving surgical treatment for CRC in the Department of Oncology and Radiotherapy of Golestan Hospital in Ahvaz City located in South-West Iran between 2001 and 2010.
Methods and Materials:
All patients who underwent resection for CRC by open or laparoscopic approaches were included in the study. Data were collected from patients’ medical records.
Statistical Analysis Used:
Statistical data were analyzed using SPSS 21.
Results:
A total of 585 cases with CRC aged from16 to 89 years with mean age of 53-year-old were studied. Average number of dissected nodes was 8 lymph nodes, and lymph nodes were not found in pathology specimen of 61 cases (10.4%). In 199 patients (34.01%), number of dissected lymph nodes was 12 or more and in 386 patients (65.98%), number of dissected lymph nodes was < 12.
Conclusion:
This study revealed a large amount of patients that had been under over treatment with radiotherapy and the following inability. Lack of removal of sufficient tissue by the surgeon during surgery or an inadequate sample check by a pathologist might lead to an inability to correct staging of the disease as well as the inability to determine the treatment program of the patients and over treatment with radiotherapy and chemotherapy.
INTRODUCTION
Cancer is an emerging and major common public health problem in developing countries.[1] Colorectal cancer (CRC) has considerable morbidity and mortality, with more than 1000,000 new cases and 500,000 annual deaths.[2] This malignancy is considered as the third common cancer in both men and women associated with advancing age, lifestyle, and environmental factors imposing a serious demographic and economic burden worldwide.[1,3,4] The International American Joint Committee on Cancer tumor node metastasis staging system is currently considered as the most powerful prognostic parameter for CRC patients.[5] The most common sites of metastasis from colon cancer are the regional lymph nodes, liver, lung, and the peritoneum.[6,7] Lymph node metastasis carries enormous prognostic weight in the evaluation of colon cancer and extension of lymph node dissection.[8,9] Surgical resection of the primary and regional lymph nodes is still, at this time, the standard treatment of colon cancer.[10] There has been considerable discussion in the literature regarding the importance and validity of lymph node retrieval and lymph node count for patients with colon cancer.[11] Lymph node dissection has several goals:
- Staging of cancer at the time of intervention;
- Improving the chances for complete resection and cure;
- Evaluating the thoroughness and quality of a particular surgical procedure.[9]
METHODS
We conducted a retrospective study among patients receiving surgical treatment for CRC in the Department of Oncology and Radiotherapy of Golestan Hospital in Ahvaz City located in South-West Iran between 2001 and 2010. All patients who underwent resection for CRC by open or laparoscopic approaches were included in the study. Data were collected from patients’ medical records. Data points included age, tumor stage, total number of lymph nodes recovered, number of lymph nodes involved, and type of surgical approach. The choice of the surgical approach was at the discretion of the surgeon. Approval from the Ethic Committee of Ahvaz Jundishapur University of Medical Sciences was obtained before data collection and review. Statistical data were analyzed using SPSS version 21.
RESULTS
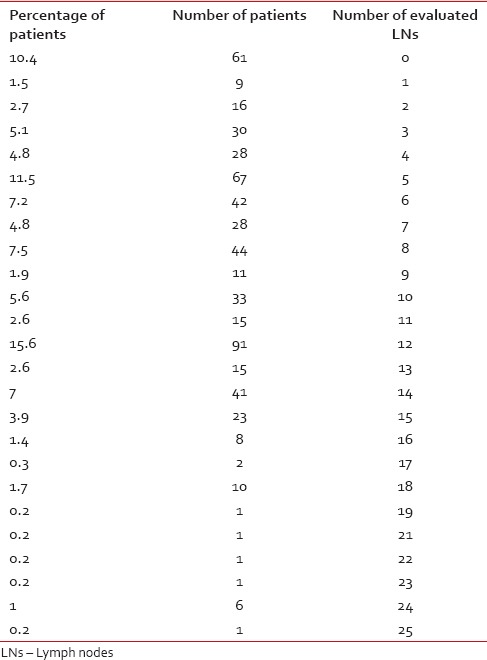
A total of 585 cases with CRC aged from16 to 89 years with mean age of 53-year-old were studied. Out of them, 330 patients (56.41%) were male and 255 patients (43.59%) were female. Most common age for CRC was 41-60-year-old in this study with 44.44% of patients in this age group. The least common age group was 0-20 years old with 1.5% of patients. Patients data in different years is summarized in Table 1. Number and percentage of patients with different number of dissected lymph nodes are summarized in Table 2. Average number of dissected nodes was 8 lymph nodes, and lymph nodes were not found in pathology specimen of 61 cases (10.4%). In 199 patients (34.01%), number of dissected lymph nodes was 12 or more and in 386 patients (65.98%), number of dissected lymph nodes was < 12.
Table 1
Results of study during 2001-2009
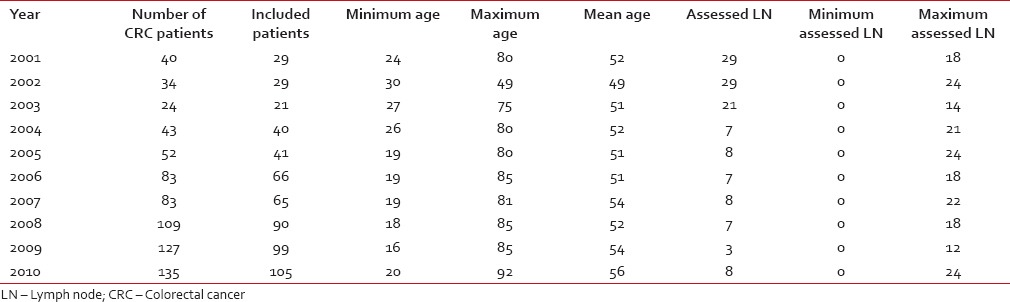
Table 2
Number and percentage of patients with different number of dissected lymph nodes
Number and percentage of patients with different number of involved lymph nodes are summarized in Table 3. Average number of involved nodes was 7 lymph nodes.
Table 3
Number and percentage of patients with different number of involved lymph nodes
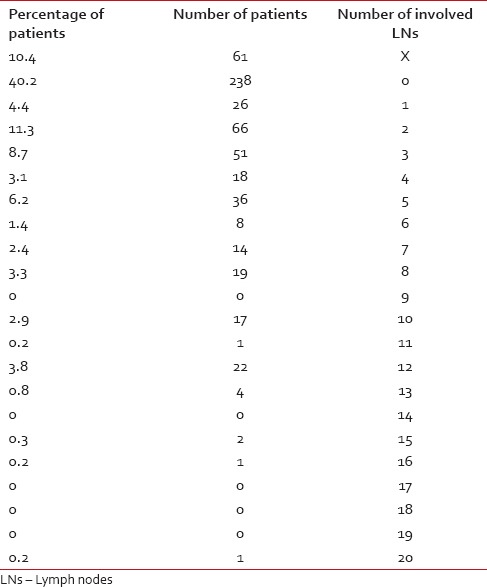
In 386 patients with < 12 dissected lymph nodes, 40.40% had no involved lymph nodes and 15.8% had unknown number of involved lymph nodes. Percentage of involved lymph nodes in patients with < 12 dissected lymph nodes are summarized in Chart 1.
DISCUSSION
Surgical resection is the mainstay of treatment for CRC with curative intent.[12] Lymph node assessment following CRC operation has received a lot of attention. The lymph node counts are really more associated with the surgeon and pathologist than on the approach.[13] Some studies have demonstrated that female gender is a significant independent predicting factor in decreasing lymph nodes involvement. Our study did not show that sex would significantly influence the total number of lymph nodes recovered or the number of involved lymph nodes.
During 2001-2010 the refereed patients with CRC increased that it can be due to familiarity of more people with symptoms of CRC as well as diagnostic facilities and more incidence of the CRC compared to past years.
Average age of CRC incidence is ≥50 years.[2] According to our study, the frequency of CRC in patients older 40 years was 77% (550 patients). This finding is consistent with previous studies that have reported the more frequency of incidence of CRC in patients older than 50 years.[2,14] In our study, the patients with CRC were 56.41% male and 43.59% female.
The number of involved lymph nodes is the most important and most effective factor in determining the prognosis and treatment plan that have been mentioned in studies of Jass and the International Association of Colon and Breast Surgery.[6,7,15]
In the current study, the average of lymph node counts was 8 lymph nodes. The investigated lymph nodes were 12 with 199 cases (33.68%). The maximum assessed lymph nodes were just in one case which contains 25 nodes, and there were not any dissected lymph nodes in 61 cases (10.4%). The maximum reported metastasized lymph node was 20 (also in one case) and minimum metastasized lymph node was 0 in 238 cases (40.2%). There were 217 patients (42.5% in total cases) with < 12 lymph nodes involvement and without metastasized lymph nodes. This means a large amount of patients that had been under over treatment with radiotherapy and the following inability.
Lack of removal of sufficient tissue by the surgeon during surgery or an inadequate sample check by a pathologist might lead to an inability to correct staging of the disease as well as the inability to determine the treatment program of the patients and over treatment with radiotherapy and chemotherapy.
Our study contains limitations. The retrospective nature of this study is a limiting factor. We were also unable to control for possible differing pathologic preparations of our specimen.
Recommendations
- Removing the appropriate amount of tissue by surgeons during surgery and checking more amount of tissue by the pathologist to determine the involved lymph nodes and minimize adjuvant treatments.
- A study must be performed on determining the longevity and survival of these patients after treatments completed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.


 PDF
PDF  Views
Views  Share
Share

