A Report of a Rare Case of Hurthle Cell Carcinoma of Thyroid with Metachronous Renal Metastasis
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(03): 409-411
DOI: DOI: 10.4103/ijmpo.ijmpo_147_18
Abstract
Renal metastasis from Hurthle cell thyroid carcinoma is an extremely rare phenomenon which when present usually indicates widely disseminated disease. Herein, we present a case of Hurthle cell carcinoma of thyroid in a 58-year-old gentle lady, with metachronous renal metastasis which happens to be the fourth reported case in English literature.
Publication History
Received: 06 July 2018
Accepted: 12 September 2018
Article published online:
28 June 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Renal metastasis from Hurthle cell thyroid carcinoma is an extremely rare phenomenon which when present usually indicates widely disseminated disease. Herein, we present a case of Hurthle cell carcinoma of thyroid in a 58-year-old gentle lady, with metachronous renal metastasis which happens to be the fourth reported case in English literature.
Introduction
Hurthle cell carcinoma is a rare variant of follicular carcinoma of thyroid, accounting for about 3%-of all thyroid malignancies.[1] These tumors tend to recur locoregionally, and distant metastases are rather uncommon.[2] However, distant failure represents the most frequent cause of thyroid cancer-related death in these patients. The most common sites of metastases encountered are lungs and bones.[3] Renal metastasis is extremely rare. Herein, we present a case of Hurthle cell carcinoma of thyroid with metachronous renal metastasis. Extensive literature search suggests it to be the fourth reported case.[2],[4],[5]
Case Report
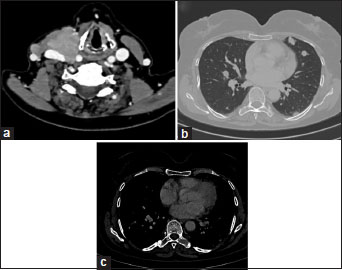
An otherwise well, 58-year-old lady presented with swelling in the right side of the neck for 3 years in December 2014 which was rapidly progressing for the past 3 months. Contrast-enhanced computed tomography (CECT) scan of the neck, thorax, and abdomen revealed a large heterogeneous mass in the right lobe of thyroid with no evidence of distant metastasis. Fine-needle aspiration cytology from swelling showed predominantly Hurthle cells. She underwent total thyroidectomy in January 2015. Histopathologic examination of postoperative specimen showed features of Hurthle cell carcinoma [Figure 1]. Tumor was seen involving capsule, surrounding soft tissue, skeletal muscle, and skin. Six lymph nodes (two each from paratracheal, Level III, and central lymph nodes) were dissected which were all involved by tumor. She was started on levothyroxine and underwent Iodine-131 whole-body scan, 6-week postsurgery, which showed thyroid remnant, left cervical Level VI lymph node, and bilateral pulmonary nodules. Hence, she was administered 150 mCi radioiodine (RAI) therapy thrice at 6-month intervals till April 2016. Post-third session therapy and Iodine-131 whole-body scan showed faint uptake in the right neck node. In December 2016, she developed a right cervical swelling in the neck, and on Iodine-131 whole-body scan, there was no uptake. CECT scan of the neck, thorax, and abdomen was done which showed multiple right cervical lymph nodes at Level II, III, IV and supraclavicular region, bilateral pulmonary nodules, and lytic destruction of left transverse process of D8 vertebra [Figure 2]. A large exophytic lesion (40 mm × 29 mm) was seen arising from the posterior interpolar region of the right kidney suggestive of renal metastasis [Figure 3]. Thyroglobulin was measured 2625 ng/ml. She was administered palliative radiotherapy of 20 gray (Gy) in five fractions over 1 week to the neck and 8 Gy in single fraction to D7–D9 vertebrae. Subsequently, she was started on oral sorafenib in view of progressive disease.
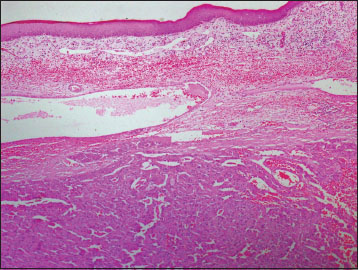
| Figure 1:Histopathologic examination showing features of Hurthle cell carcinoma
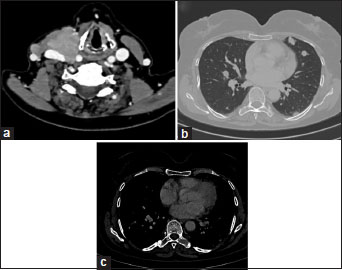
| Figure.2:Contrast-enhanced computed tomography scan showing right cervical lymph nodes (a), bilateral pulmonary nodules (b), and lytic destruction of left transverse process of D8 vertebra (c)

| Figure.3:Contrast-enhanced computed tomography scan showing right renal metastasis
Discussion
According to the World Health Organization classification, Hurthle cell thyroid carcinoma (HCTC) is considered to be an oxyphilic variant of follicular thyroid carcinoma (FTC).[6] Although earlier studies reported inferior survival of these patients with HCTC,[7] a recent study by Bhattacharyya[1] showed similar outcome as compared with patients of FTC. However, it has been seen that HCTC is associated with higher rates of metastases compared to other subtypes. Lung and bone are the most common sites of distant metastases.[3] Renal metastasis is a rare occurrence. Exhaustive search of English literature revealed that our presented case is the fourth case reported [Table 1]. In general, metastatic kidney lesion should ideally be proven by biopsy, but the diagnosis by imaging may also be acceptable in cases where the lesion is too small to be biopsied or biopsy is not possible due to medical comorbidities.[4] In the index case, biopsy from the renal lesion was not done in view of strong clinicoradiological correlation. Treatment of metastatic HCTC is not well defined owing to its low incidence and hence fewer extensive experience. The management of distant metastases includes levothyroxine replacement, focal therapy, and systemic treatment (including RAI), and in patients with RAI-refractory disease, it includes the use of kinase inhibitors. Focal treatment is indicated in local tumor palliation and orthopedic or neurologic sequelae, for example, external beam radiotherapy (EBRT) for palliation of the bone and brain metastasis or surgical fixation for fractures. RAI ablation is difficult in HCTC as most of them do not uptake RAI, and some of the tumors which show faint uptake is probably due to the follicular component.[3] Chemotherapy is usually not effective.[8] Among kinase inhibitors, sorafenib is approved by the US Food and Drug Administration for advanced differentiated thyroid cancer.[9] Similarly, our patient was managed by sorafenib and local EBRT to the neck and D8 vertebrae.
|
Authors |
Age (years) |
Sex |
Renal metastasis diagnosed by |
Treatment received |
|---|---|---|---|---|
|
CT – Computed tomography; RAI – Radioiodine; SPECT – Single-photon emission computed tomography; FDG – Fluoro-deoxyglucose |
||||
|
Djekidel et al.[1] |
75 |
Male |
FDG positron emission tomography-CT scan, magnetic resonance imaging |
Thyroidectomy, RAI therapy, radical nephrectomy, and palliative radiotherapy to vertebral metastasis |
|
Claimon et al.[4] |
61 |
Female |
SPECT/CT imaging |
Thyroidectomy and RAI therapy |
|
Kushchayeva et al.[6] |
70 |
Unknown |
Unknown |
Thyroidectomy, RAI therapy, and radical nephrectomy |
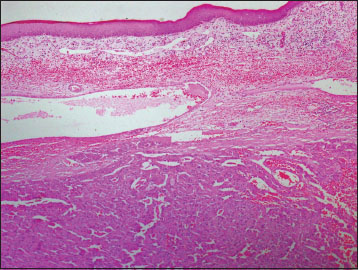
| Figure 1:Histopathologic examination showing features of Hurthle cell carcinoma
| Figure.2:Contrast-enhanced computed tomography scan showing right cervical lymph nodes (a), bilateral pulmonary nodules (b), and lytic destruction of left transverse process of D8 vertebra (c)

| Figure.3:Contrast-enhanced computed tomography scan showing right renal metastasis
References
- Bhattacharyya N. Survival and prognosis in Hürthle cell carcinoma of the thyroid gland. Arch Otolaryngol Head Neck Surg 2003; 129: 207-10
- Djekidel M, Gordon M, Shah RB, Gross MD, Avram A. Renal metastasis from Hurthle cell thyroid carcinoma and its evaluation with hybrid imaging. Thyroid 2010; 20: 429-33
- Zhang H, Zeng L, Liang C, Qiu H, Zhang M, Zhu Y. et al. Successful treatment of Hurthle cell thyroid carcinoma with lung and liver metastasis using docetaxel and cisplatin. Jpn J Clin Oncol 2012; 42: 1086-90
- Claimon M, Suh M, Cheon GJ, Lee DS, Kim EE, Chung JK. et al. Bilateral renal metastasis of Hürthle cell thyroid cancer with discordant uptake between I-131 sodium iodide and F-18 FDG. Nucl Med Mol Imaging 2017; 51: 256-60
- Besic N, Schwarzbartl-Pevec A, Vidergar-Kralj B, Crnic T, Gazic B, Marolt Music M. et al. Treatment and outcome of 32 patients with distant metastases of Hürthle cell thyroid carcinoma: A single-institution experience. BMC Cancer 2016; 16: 162
- Kushchayeva Y, Duh QY, Kebebew E, Clark OH. Prognostic indications for Hürthle cell cancer. World J Surg 2004; 28: 1266-70
- Watson RG, Brennan MD, Goellner JR, van Heerden JR, McConahey WM, Taylor WF. et al. Invasive Hürthle cell carcinoma of the thyroid: Natural history and management. Mayo Clin Proc 1984; 59: 851-5
- Lopez-Penabad L, Chiu AC, Hoff AO, Schultz P, Gaztambide S, Ordoñez NG. et al. Prognostic factors in patients with Hürthle cell neoplasms of the thyroid. Cancer 2003; 97: 1186-94
- Haugen BR, Sherman SI. Evolving approaches to patients with advanced differentiated thyroid cancer. Endocr Rev 2013; 34: 439-55


 PDF
PDF  Views
Views  Share
Share

