A rare cause for hematuria: Lymphoma of the urinary bladder
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(05): 764-766
DOI: DOI: 10.4103/ijmpo.ijmpo_224_19
Abstract
Primary lymphomas of the urinary bladder are rare and majority present with hematuria. Patients are usually elderly females with a history of recurrent cystitis. The diagnosis is clinched after imaging and biopsy of suspicious lesions in the bladder. The prognosis is good irrespective of the modality of treatment. With this background, we report a case of primary marginal zone lymphoma of the urinary bladder (Stage IE) in a young lady with no history of cystitis, who presented with isolated hematuria. After treatment with radiotherapy alone, patient is in complete remission for the past 18 months. The timely diagnosis in a patient with hematuria holds the key to successful treatment and its importance cannot be overemphasized.
Keywords
Hematuria - marginal zone lymphoma - mucosa-associated lymphoid tissue - primary lymphoma - radiotherapy - urinary bladderPublication History
Received: 03 November 2019
Accepted: 15 March 2020
Article published online:
17 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Primary lymphomas of the urinary bladder are rare and majority present with hematuria. Patients are usually elderly females with a history of recurrent cystitis. The diagnosis is clinched after imaging and biopsy of suspicious lesions in the bladder. The prognosis is good irrespective of the modality of treatment. With this background, we report a case of primary marginal zone lymphoma of the urinary bladder (Stage IE) in a young lady with no history of cystitis, who presented with isolated hematuria. After treatment with radiotherapy alone, patient is in complete remission for the past 18 months. The timely diagnosis in a patient with hematuria holds the key to successful treatment and its importance cannot be overemphasized.
Keywords
Hematuria - marginal zone lymphoma - mucosa-associated lymphoid tissue - primary lymphoma - radiotherapy - urinary bladderIntroduction
Primary lymphomas of the urinary bladder are rare, representing 0.2% of all known bladder cancers.[1] The most common symptoms of bladder lymphomas are macroscopic hematuria, dysuria, and increased frequency of micturition.[2] In the literature reported so far, patients are usually elderly and have a history of chronic cystitis. Herein, we report a case of a young female with no such history, who is in complete remission after treatment.
Case Report
A 35-year-old lady with no comorbidity presented to the urologist with 1-month history of painless hematuria. On physical examination, no pallor, lymphadenopathy, hepatosplenomegaly, or any mass in the pelvis was detected. The urine routine and microscopic examination was confirmative of hematuria. Thereafter, a contrast-enhanced computed tomography (CECT) of the abdomen and pelvis showed a large, lobulated mass, 96 mm × 46 mm × 63 mm, in the posterolateral wall of the urinary bladder with few subcentimeters internal iliac and left obturator lymph nodes. The mass was encasing the left vesicoureteral junction causing mild proximal hydroureteronephrosis [Figure 1] and [Figure 2].

| Figure 1: Contrast enhanced computed tomography of the abdomen and pelvis showing the tumor arising from the posterolateral bladder wall – Coronal section

| Figure 2: Axial section of the same contrast enhanced computed tomography showing the tumor
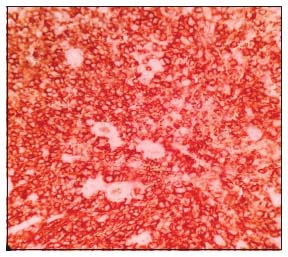
Subsequently, cystoscopy showed a well-defined, lobulated submucosal mass arising from the posterior wall from which biopsy was taken. Histopathological examination of the biopsy specimen revealed infiltration of the bladder mucosa by sheets of monomorphic population of small, atypical lymphocytes, suggestive of non-Hodgkin's lymphoma [Figure 3].
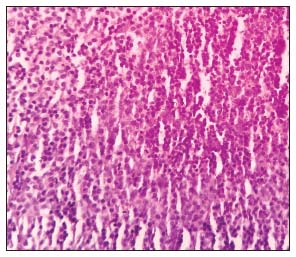
| Figure 3: Atypical lymphocytes infiltrating the submucosa of the urinary bladder (H and E, ×40)
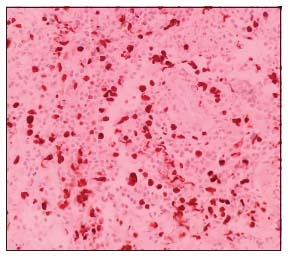
The immunohistochemistry was positive for leucocyte common antigen and also for CD20, [Figure 4] Bcl2, CD5, CD43, CD68, and MPO. About 40% of cells stained positive for MIB-1 [Figure 5]. CD10 and cyclin D1 were negative, consistent with marginal zone B-cell lymphoma (MZL) with a high proliferative index.
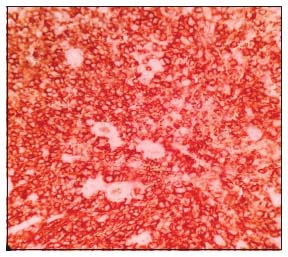
| Figure 4: The tumor cells staining for CD20 on immunohistochemistry (×40)
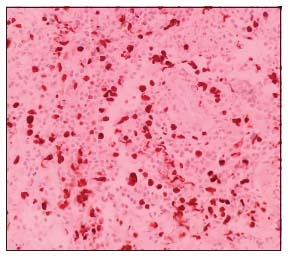
| Figure 5: MIB‑1 positivity among 40% of tumor cells (×40)
The patient had a hemoglobin of 11.5 g/dl and total leukocyte count of 5500/mm3 with 78% neutrophils and platelet count of 3.5 lakhs/mm3. Her lactate dehydrogenase was 139 U/L. Bone marrow aspiration and trephine bone biopsy did not show infiltration by lymphoma and CECT of the neck and thorax showed no disease elsewhere. Hence, the final diagnosis of primary MZL of the urinary bladder stage IE was confirmed.
In view of localized disease, the patient was treated with curative intent, by means of radiation therapy of 50 Gy in 25 fractions. She tolerated the therapy well with no major side effects following which the hematuria subsided. A repeat CECT of the pelvis showed soft-tissue density lesion with a size of 21 mm × 37 mm × 32 mm at the base of the urinary bladder – presumably residual disease or postradiation changes. After 2 months, it had reduced to a size of 17 mm × 35 mm, and cystoscopic guided biopsy was negative for malignancy. She is under observation with CECT pelvis and urine cytology now. Her recurrence-free survival is 18 months.
Discussion
Since the first report of primary lymphosarcoma of the urinary bladder by Eve in 1885,[2] much has come to light about this rare lymphoma. It was classified along with sarcomas and the treatment has evolved from surgery alone to adjuvant radiotherapy and then to multimodality therapy.
Extranodal marginal zone lymphomas or mucosa-associated lymphoid tissue (MALT) lymphomas were first described by Isaacson in 1983 where he postulated the MALT concept to explain the development of lymphomas in organs with no lymphoid tissues.[1] This concept of acquisition of lymphoid tissue due to chronic antigenic stimulation by a bacterial infection is supported by the history of chronic cystitis, seen in around 20%–40% of the cases.[3] On the other hand, in those cases with no such previous history, like ours, the alternative hypothesis is the development of tumors from the lymphoid tissue derived from the embryonic cloaca.[2]
Extranodal marginal zone lymphomas are most common among primary urinary bladder lymphomas. More than 50 cases of primary bladder marginal zone lymphomas have been reported so far, after the first by Kuhara et al. in 1990.[4] Patients are mostly elderly females, more than 60 years of age, with a history of chronic cystitis in the past, contrary to the patient reported here. Hematuria was the predominant symptom in 60%, with others having dysuria and urinary frequency.[2]
Since there is no consensus on the optimal therapy, either of radiation, chemotherapy, targeted therapy, or a combination have been attempted and are successful in attaining remission. A few patients were treated with local therapy only, such as transurethral resection of bladder tumor[5] and diathermy. There was one patient who attained CR with Helicobacter pylori eradication therapy alone,[6] while another patient was treated exclusively with rituximab.[2] In this context, all cases reported after 2014 are shown in [Table 1]. The prognosis remains good despite the modality of treatment used, but rarely, it can disseminate or transform into higher grade diffuse large B-cell lymphoma.[2],[7]
Table 1 All cases of marginal zone B-cell lymphoma urinary bladder reported since 2014
Conclusion
Although marginal zone lymphoma of the bladder is not a common diagnosis of a patient with hematuria, hematuria is its most common presentation. Hence, urine cytology and cystoscopy should be done in persistent cases of hematuria to rule out the same, as it has a very good prognosis with any form of either local or systemic therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflict of Interest
There are no conflicts of interest.
Acknowledgment
The authors are grateful to the Department of Pathology, Gujarat Cancer and Research Institute for the photomicrographs.
References
- D'Souza N, Verma A, Rai A. Two cases of non-Hodgkin lymphoma of urinary bladder: Primary and secondary. J Cancer Res Ther 2017; 13: 1053-5
- Combaz N, Kuhn A. Case report about a primary bladder lymphoma. Int Arch Urol Complicat 2017; 3: 1-6
- Isono M, Sato A, Kimura F, Asano T. A case of mucosa-associated lymphoid tissue lymphoma of the bladder successfully treated with radiotherapy. Urol Case Rep 2018; 16: 1-3
- Kuhara H, Tamura Z, Suchi T, Hattori R, Kinukawa T. Primary malignant lymphoma of the urinary bladder. A case report. Acta Pathol Jpn 1990; 40: 764-9
- Ozawa M, Suenaga S, Ishii T, Suzuki H, Tsuchiya N, Ohtake H. Primary malignant lymphoma of the bladder diagnosed by transurethral bladder tumor resection: A case report. Nihon Hinyokika Gakkai Zasshi 2018; 109: 45-9
- van den Bosch J, Kropman RF, Blok P, Wijermans PW. Disappearance of a mucosa-associated lymphoid tissue (MALT) lymphoma of the urinary bladder after treatment for Helicobacter pylori. Eur J Haematol 2002; 68: 187-8
- Matsuda I, Zozumi M, Tsuchida YA, Kimura N, Liu NN, Fujimori Y. et al. Primary extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue type with malakoplakia in the urinary bladder: A case report. Int J Clin Exp Pathol 2014; 7: 5280-4
- Haddad-Lacle JE, Haddad CJ, Villas B. A rare urinary bladder tumour. BMJ Case Rep [Internet]. 2014 https://casereports.bmj.com/content/2014/bcr-2013-202994.long. May, 2014:bcr2013202994:[about 2p.]. Available from: [Last cited 2019 Oct 17]
- Chen YR, Hung LY, Chang KC. Mucosa-associated lymphoid tissue-type lymphoma presenting as a urethral caruncle with urinary bladder involvement. Int J Urol 2014; 21: 1073-4
- Hsu JS, Lin CC, Chen YT, Lee YC. Primary mucosa-associated lymphoid tissue lymphoma of the urinary bladder. Kaohsiung J Med Sci 2015; 31: 388-9
Address for correspondence
Publication History
Received: 03 November 2019
Accepted: 15 March 2020
Article published online:
17 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India

| Figure 1: Contrast enhanced computed tomography of the abdomen and pelvis showing the tumor arising from the posterolateral bladder wall – Coronal section

| Figure 2: Axial section of the same contrast enhanced computed tomography showing the tumor
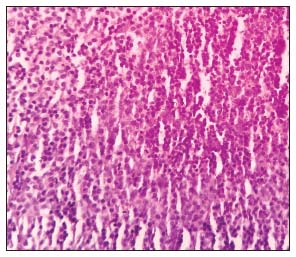
| Figure 3: Atypical lymphocytes infiltrating the submucosa of the urinary bladder (H and E, ×40)
| Figure 4: The tumor cells staining for CD20 on immunohistochemistry (×40)
| Figure 5: MIB‑1 positivity among 40% of tumor cells (×40)
- 1 D'Souza N, Verma A, Rai A. Two cases of non-Hodgkin lymphoma of urinary bladder: Primary and secondary. J Cancer Res Ther 2017; 13: 1053-5
- 2 Combaz N, Kuhn A. Case report about a primary bladder lymphoma. Int Arch Urol Complicat 2017; 3: 1-6
- 3 Isono M, Sato A, Kimura F, Asano T. A case of mucosa-associated lymphoid tissue lymphoma of the bladder successfully treated with radiotherapy. Urol Case Rep 2018; 16: 1-3
- 4 Kuhara H, Tamura Z, Suchi T, Hattori R, Kinukawa T. Primary malignant lymphoma of the urinary bladder. A case report. Acta Pathol Jpn 1990; 40: 764-9
- 5 Ozawa M, Suenaga S, Ishii T, Suzuki H, Tsuchiya N, Ohtake H. Primary malignant lymphoma of the bladder diagnosed by transurethral bladder tumor resection: A case report. Nihon Hinyokika Gakkai Zasshi 2018; 109: 45-9
- 6 van den Bosch J, Kropman RF, Blok P, Wijermans PW. Disappearance of a mucosa-associated lymphoid tissue (MALT) lymphoma of the urinary bladder after treatment for Helicobacter pylori. Eur J Haematol 2002; 68: 187-8
- 7 Matsuda I, Zozumi M, Tsuchida YA, Kimura N, Liu NN, Fujimori Y. et al. Primary extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue type with malakoplakia in the urinary bladder: A case report. Int J Clin Exp Pathol 2014; 7: 5280-4
- 8 Haddad-Lacle JE, Haddad CJ, Villas B. A rare urinary bladder tumour. BMJ Case Rep [Internet]. 2014 https://casereports.bmj.com/content/2014/bcr-2013-202994.long. May, 2014:bcr2013202994:[about 2p.]. Available from: [Last cited 2019 Oct 17]
- 9 Chen YR, Hung LY, Chang KC. Mucosa-associated lymphoid tissue-type lymphoma presenting as a urethral caruncle with urinary bladder involvement. Int J Urol 2014; 21: 1073-4
- 10 Hsu JS, Lin CC, Chen YT, Lee YC. Primary mucosa-associated lymphoid tissue lymphoma of the urinary bladder. Kaohsiung J Med Sci 2015; 31: 388-9


 PDF
PDF  Views
Views  Share
Share

