A rare case of peripheral T-cell lymphoma in 1-year-old child
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2011; 32(04): 227-229
DOI: DOI: 10.4103/0971-5851.95147
Abstract
Peripheral T-cell lymphoma (PTCL) represents approximately 12% of lymphoid neoplasms. They are even rarer in children and represent only 1% of Non-Hodgkin′s lymphoma in this age group. We report a case of PTCL in a 1-year-old female child for its rarity.
Keywords
ALK negative anaplastic T-cell lymphoma - peripheral T-cell lymphoma - non-Hodgkin lymphoma - unusual chemoresponsPublication History
Article published online:
06 August 2021
© 2011. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Peripheral T-cell lymphoma (PTCL) represents approximately 12% of lymphoid neoplasms. They are even rarer in children and represent only 1% of Non-Hodgkin's lymphoma in this age group. We report a case of PTCL in a 1-year-old female child for its rarity.
Lymphomas are the third most common pediatric malignancy constituting 10% of cancer in children, of which two-thirds are non-Hodgkin's lymphoma (NHL).[1] Four commonest type of NHL in children are Lymphoblastic lymphoma, Burkitt's lymphoma, Anaplastic large-cell lymphoma, and diffuse large B-cell lymphoma.[2] Peripheral T-cell lymphomas (PTCLs) are rare in childhood and represent only 1% of NHL cases.[3] Their response to conventional chemotherapy is indeed poor, with 5-year relapse-free and overall survival rates of 26% and 20%, respectively.[4] Conventional morphological and molecular criteria do not assist in the subclassification of PTCL/not otherwise specified (NOS).
A 1-year-old female child presented with fever and abdominal distention of 2-month duration. On examination, the child was febrile, had generalized lymphadenopathy including retroperitoneal lymph nodes and hepatosplenomegaly.
Investigations revealed raised white blood corpuscle count (15×109/l with lymphocytes 66%), high lactate dehydrogenase - 712 IU/l. Her hemoglobin, platelet, fibrinogen, renal function test, liver function test, serum uric acid, and serum electrolytes were normal. Cerebro spinal fluid analysis did not reveal any abnormal cells. Contrast-enhanced computed tomography scan (CECT) of thorax showed an enlarged thymus in superior mediastinum along with enlarged lymph nodes in right paratracheal, subcarinal, bilateral axillary, and bilateral cervical regions. CECT abdomen and pelvis revealed hepatosplenomegaly, large retroperitoneal lymph node mass of 8×7 cm encasing the abdominal vessels. Cervical lymph node biopsy revealed partial effacement of architecture with proliferation of large, round to polygonal cells with moderate cytoplasm, and large irregular vesicular nuclei with prominent nucleoli were seen. Increased mitosis was present. Lymphatic spaces also showed atypical cells. Immunohistochemistry: Leukocyte common antigen, CD3 [Figure 1], CD43 [Figure 2], Bcl2 and CD57 positive. CD30, terminal deoxynucleotidyl transferase, anaplastic lymphoma kinase-1, CD56, UCHL-1, CD20, CD79α, epithelial membrane antigen, CD15, CD10, MPO, and CD68 negative.
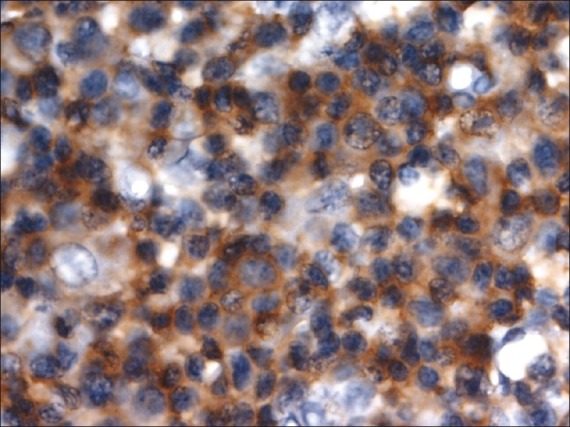
| Figure 1:PTCL unspecified showing CD3 expression
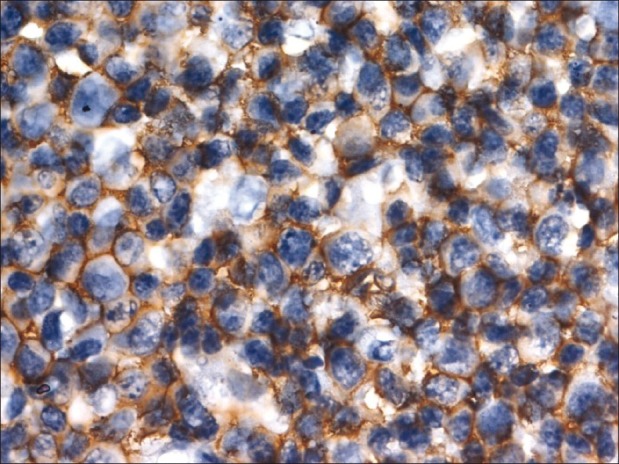
| Figure 2:PTCL unspecified showing CD43 expression
The Ki 67 labelling of atypical cells was 65%. Bone marrow was infiltrated by atypical lymphoid cells. Based on these, a diagnosis of Stage IV PTCL was made. Patient was started on MCP 842 protocol chemotherapy. This protocol contains alternating cycles of Regimen A and Regimen B. The patient completed eight cycles of chemotherapy, achieved complete remission, and remained disease free at 6 months of follow-up.
DISCUSSION
T-cell lymphomas other than analplastic large cell lymphoma and Lymphoblastic lymphomas in children are extremely rare diseases and are essentially uncharacterized, except as case reports and anecdotes. Only 1 case of infantile PTCL-NOS was reported over a 20 year period from a National child hood registry.[5] It has been suggested that a majority tend to be derived from components of the innate immune system including cytotoxic T or NK cells.[6] Their prognosis is not known and their occurrence results in confusion regarding choice of therapy.
Other sujbtypes of PTCL are equally rare and published only as case reports.[7]
However, the response to treatment is often poor and the relapse rate is high.[8] The role of autologous transplant is pediatric PTCL is unclear.[9] At present, treatment for PTCL NOS is unsatisfactory.
Data about PTCL from adult population suggest an inferior response to chemotherapy and poorer outcomes compared with age- and stage-matched diffuse large B-cell lymphomas (the other common aggressive lymphoma in adults), when treated with adult protocols.[10] Since there are limited data in children on this entity, we decided to treat this patient with an aggressive pediatric lymphoma protocol. Despite having a high-risk disease with extensive bone marrow involvement, and bulky abdominal nodes, this child had a very satisfactory response and remains disease free. Though more aggressive approaches to treating PTCL in adults have been postulated including the use of high-dose therapy as consolidation, this approach remains controversial as yet. This report of a rare disease in a child seems to suggest that an aggressive approach might be effective in PTCL of childhood.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- Shukla NN, Trippett TM. Non Hodgkins lymphoma in children and young adolescents. Curr Oncol Rep 2006;8:387.
- Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, et al. A revised European - American Classification of lymphoid neoplasms; a proposal from International Lymphoma Study Group. Blood 1994;84:1361-92.
- Reiter A, Schrappe M, Parwaresch R, Henze G, Müller-Weihrich S, Sauter S, et al. Non-Hodgkin′s lymphomas of childhood and adolescence: Results of a treatment stratified for biologic subtypes and stage- a report of Berlin-Frankfurt -Munster group. J Clin Oncol 1995;13: 359-72.
- Gallamini A, Stelitano C, Calvi R, Bellei M, Mattei D, Vitolo U, et al. Peripheral T-Cell lymphoma unspecified: A new prognostic model from a retrospective multicentric clinical study. Blood 2004;103:2474-9.
- Windsor R, Stiller C, Webb D. Peripheral T-Cell lymphoma in childhood: Population-based experience in the United Kingdom over 20 years. Pediatr Blood Cancer 2008;50: 784-78.
- Jaffe ES. MatureT-cell and NK-cell lymphomas in the pediatric age group. Am J Clin Pathol 2004;122:S110-21.
- Hutchison RE, Laver JH, Chang M, Muzzafar T, Desai S, Murphy S, et al. Non-anaplastic peripheral T-cell lymphoma in childhood and adolescence: A Children′s Oncology Group study. Pediatr Blood Cancer 2008;51:29-33.
- Mounier N, Simon D, Haioun C, Gaulard P, Gisselbrecht C. Impact of high dose chemotherapy on peripheral T-cell lymphoma. J Clin Oncol 2002;5:1426-7.
- Beresford MW, Wilkins S, Ashworth M, Davidson JE, McDowell H, Cleary AG. Peripheral T-Cell lymphoma in a five year old. Pediatr Blood Cancer 2008;50:145-7.
- Savage KJ. Aggressive peripheral T-Cell lymphomas (Specifed and unspecified types). Hematology Am Soc Hematol Educ Program 2005;267-77.
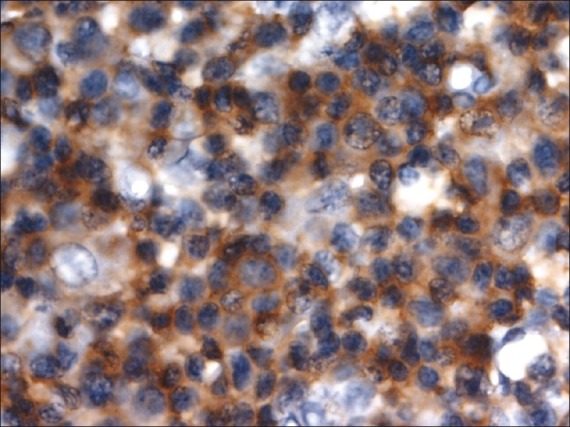
| Figure 1:PTCL unspecified showing CD3 expression
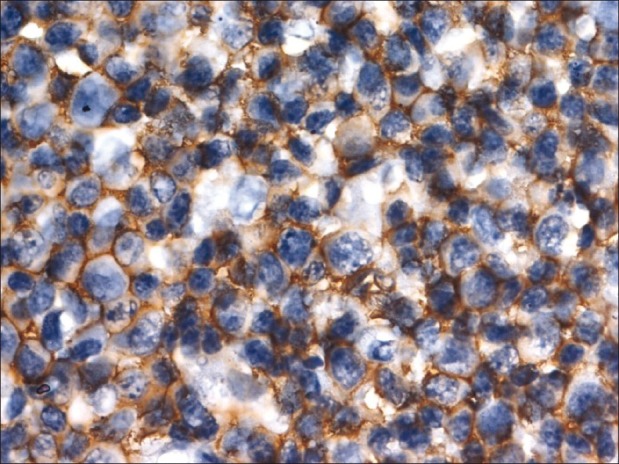
| Figure 2:PTCL unspecified showing CD43 expression
References
- Shukla NN, Trippett TM. Non Hodgkins lymphoma in children and young adolescents. Curr Oncol Rep 2006;8:387.
- Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, et al. A revised European - American Classification of lymphoid neoplasms; a proposal from International Lymphoma Study Group. Blood 1994;84:1361-92.
- Reiter A, Schrappe M, Parwaresch R, Henze G, Müller-Weihrich S, Sauter S, et al. Non-Hodgkin′s lymphomas of childhood and adolescence: Results of a treatment stratified for biologic subtypes and stage- a report of Berlin-Frankfurt -Munster group. J Clin Oncol 1995;13: 359-72.
- Gallamini A, Stelitano C, Calvi R, Bellei M, Mattei D, Vitolo U, et al. Peripheral T-Cell lymphoma unspecified: A new prognostic model from a retrospective multicentric clinical study. Blood 2004;103:2474-9.
- Windsor R, Stiller C, Webb D. Peripheral T-Cell lymphoma in childhood: Population-based experience in the United Kingdom over 20 years. Pediatr Blood Cancer 2008;50: 784-78.
- Jaffe ES. MatureT-cell and NK-cell lymphomas in the pediatric age group. Am J Clin Pathol 2004;122:S110-21.
- Hutchison RE, Laver JH, Chang M, Muzzafar T, Desai S, Murphy S, et al. Non-anaplastic peripheral T-cell lymphoma in childhood and adolescence: A Children′s Oncology Group study. Pediatr Blood Cancer 2008;51:29-33.
- Mounier N, Simon D, Haioun C, Gaulard P, Gisselbrecht C. Impact of high dose chemotherapy on peripheral T-cell lymphoma. J Clin Oncol 2002;5:1426-7.
- Beresford MW, Wilkins S, Ashworth M, Davidson JE, McDowell H, Cleary AG. Peripheral T-Cell lymphoma in a five year old. Pediatr Blood Cancer 2008;50:145-7.
- Savage KJ. Aggressive peripheral T-Cell lymphomas (Specifed and unspecified types). Hematology Am Soc Hematol Educ Program 2005;267-77.


 PDF
PDF  Views
Views  Share
Share

