A rare case of papillary carcinoma of choroids plexus: Its management and review of literature
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2011; 32(02): 112-114
DOI: DOI: 10.4103/0971-5851.89796
Abstract
Papillary carcinoma of choroids plexus is very rare. Only a few cases have been described in the literature, and it is most commonly found in the pediatric population. A further observation is added now. A 20-year-old lady presented with complaints of headache and vomiting from past one and half months, headache was increasing in severity and there was relief after vomiting. On examination, no abnormality was detected in any of her systems. The patient underwent computed tomography scan of brain, which showed space occupying lesion in the right frontal lobe. She underwent near total excision of the lesion. Postoperative period was uneventful. Histopathology was suggestive of papillary carcinoma of choroids plexus and was confirmed with immunohistochemistry. The patient received whole brain radiation and intrathecal chemotherapy. The patient tolerated the treatment well, except for grade two vomiting. She has completed one and half years of follow-up and is disease free.
Publication History
Article published online:
06 August 2021
© 2011. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Papillary carcinoma of choroids plexus is very rare. Only a few cases have been described in the literature, and it is most commonly found in the pediatric population. A further observation is added now. A 20-year-old lady presented with complaints of headache and vomiting from past one and half months, headache was increasing in severity and there was relief after vomiting. On examination, no abnormality was detected in any of her systems. The patient underwent computed tomography scan of brain, which showed space occupying lesion in the right frontal lobe. She underwent near total excision of the lesion. Postoperative period was uneventful. Histopathology was suggestive of papillary carcinoma of choroids plexus and was confirmed with immunohistochemistry. The patient received whole brain radiation and intrathecal chemotherapy. The patient tolerated the treatment well, except for grade two vomiting. She has completed one and half years of follow-up and is disease free.
INTRODUCTION
Tumors of the choroid plexus are rare. Choroid plexus tumors account for approximately 0.4–0.6% of all brain tumors.[1] These tumors are derived from choroid plexus epithelium and characterized by papillary and intraventricular growth. Within this family of tumors, there are benign and malignant variants, typically classified as choroid plexus papilloma (CPP) and choroid plexus carcinoma (CPC), respectively.
These tumors are more common in pediatric age group (80%), representing approximately 1–4% of all childhood brain tumors, with 10–20% occurring during the first year of life, and 20–40% of all choroid plexus tumors in children are CPCs.[1] Within the pediatric population, the median age is approximately 26–32 months.[1] It has been described in association with Li-Fraumeni syndrome.[2] A study by Rickert et al. also examined the behavior of CPCs with certain chromosomal additions and deletions and concluded that tumors with a gain of 9p and loss of 10q were associated with significantly longer survival.[3] Occurrence of CPC in adults is very rare; only 16 of the 231 reported cases of CPC occurred in adults[4] and we report such a rare case.
CASE REPORT
A 20-year-old lady presented with complaints of headache and vomiting from past one and half months; headache was increasing in severity and there was relief on vomiting. She had no history of blurring or diminution of vision or seizures. There was also no history of motor or sensory disturbances. On examination, no abnormality was detected. The patient underwent computed tomography (CT) scan of brain, which showed space occupying lesion in the right frontal lobe, measuring about 6×6 cm [Figure 1]. Fundus was normal. She underwent near total excision of the lesion. Postoperative period was uneventful. Histopathology of the specimen showed features suggestive of papillary carcinoma of choroids plexus. There was increased cell density, increased mitotic figures (greater than 5 per 10 high-power fields), nuclear pleomorphism, and necrosis. Diffuse invasion of the adjacent brain parenchyma was present [Figure 2]. On immunohistochemistry, it was positive for glial fibrillary acidic protein and negative for epithelial membrane antigen [Figure 3]. Since the diagnosis of papillary carcinoma of choroid plexus is very rare in adults, patient was worked up to rule out any primary disease elsewhere in the body. Thyroid scan, chest X-ray, and ultrasonography of abdomen and pelvis were normal. Stool for occult blood was negative. Complete blood count and peripheral smear was normal. Cerebrospinal fluid (CSF) was examined for the presence of malignant cells and it was found to be negative for malignant cells. The patient received radiation to whole brain on telecobalt unit, using German helmet technique, with two lateral portals. Initial dose was 4000 cGy/20 fractions (200 cGy/fraction). Later, she received boost to the primary tumor bed, using antero-lateral wedge pair technique, to a dose of 2000 cGy/10 fractions. Along with radiation, the patient also received four cycles of intrathecal methotrexate (12 mg), cytarabine (50 mg) and hydrocortisone (20 mg) weekly. The patient tolerated the treatment well; except for grade 2 vomiting, there was no other toxicity.

| Fig. 1 CT brain showing space occupying lesion in the right frontal lobe
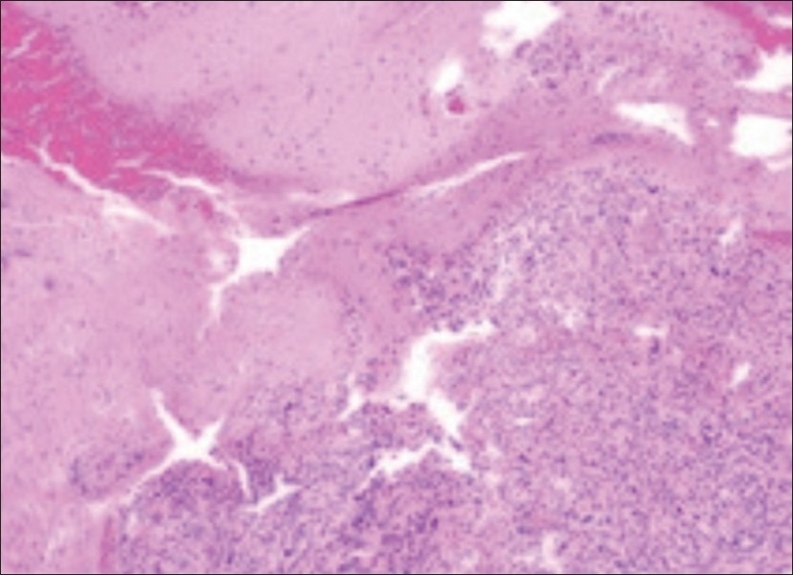
| Fig. 2 Solid sheet of choroid plexus carcinoma invading adjacent brain parenchyma (hematoxylin and eosin, original magnification ×100)
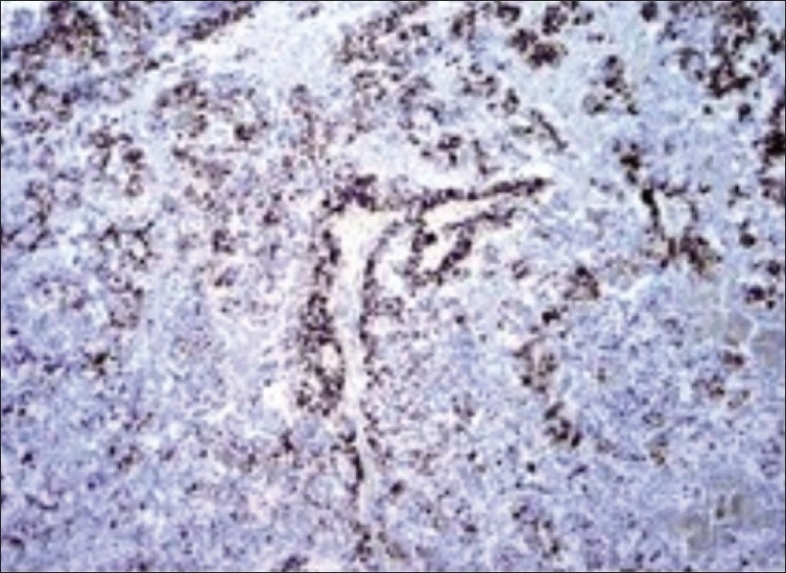
| Fig. 3 Positive glial fibrillary acidic protein staining in choroid plexus carcinoma (original magnification ×100)
DISCUSSION
CPCs present with the signs and symptoms of CSF obstruction.[1] In general, they are confined to the following: 50% to lateral ventricles, 40% to fourth ventricle, 5% to third ventricle, and 5% of multiple ventricular involvement.[1,5] Although infrequent, CPCs can occur in the cerebellopontine angle near the foramina of Lushka, and extremely rare cases may present as a suprasellar and/or intraparenchymal mass.[5,6] Seedling throughout the CSF spaces is frequent and symptomatic.
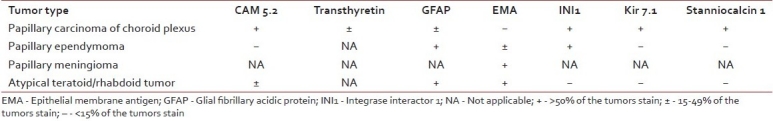
CPC must be distinguished from CPP (WHO grade I). Distinction between these entities is imperative but can be challenging, and it is generally based on increased necrosis, mitotic activity, and change in growth pattern.[7] Histopathologic features include blurring of papillary architecture, layers of neoplastic choroid plexus epithelial cells with pleomorphic nuclei, increased nuclear-to-cytoplasmic ratio, increased mitotic activity, areas of necrosis, and brain invasion,[8] whereas CPP often shows apparently normal choroid plexus, with increased cellular crowding and elongation. Proliferation indices, such as Ki-67/MIB-1, can be useful in the diagnosis of CPC, with reported mean nuclear labeling rates of 1.9% for CPP and 13.8% for CPC.[9] Immunohistochemistry must be used in order to rule out other tumors like papillary ependymoma, papillary meningioma and atypical teratoid/rhabdoid tumor [Table 1].[8]
Table 1
Immunohistochemical staining of tumors in differential diagnosis of choroid plexus carcinoma
CPCs are seen visible in magnetic resonance imaging (MRI). Imaging demonstrates a lobulated, well-circumscribed, enhancing, intraventricular lesion, often with associated hydrocephalus. Calcification is not common. Choroid carcinoma may show areas consistent with necrosis and brain invasion.[10]
Current treatment strategy consists of gross total surgical resection for both CPP and CPC; however, total resection is not possible in many patients. The ability to perform a complete resection depends on histologic type, with nearly a 100% complete resection rate for papillomas versus only a 33% complete resection rate for CPC.[11] A meta-analysis of all individual cases of CPC showed better prognosis for completely resected cases.[12] Often, tumor hypervascularity is the limiting surgical factor, especially in infants who have small total blood volumes. When carcinoma is suspected before surgery, the tumor can be embolized or neoadjuvant chemotherapy is given to shrink it and reduce its vascularity, which facilitates resection.[13]
Radiation therapy (RT) may be beneficial in patients with CPCs even after gross total resection.[14,15] Patients with completely excised CPC should be treated with limited field irradiation if their spinal MRI and CSF cytologic study results are negative. Craniospinal irradiation (CSI) is given for those with incompletely excised tumors or evidence of leptomeningeal spread.[14]
The role of adjuvant chemotherapy is not well established in CPC; in our case, the patient was treated with intrathecal methotrexate, hydrocortisone and cytarabine. The idea behind this treatment was to take care of spinal axis, as the patient was not planned for spinal RT. Though the patient did not receive any systemic adjuvant chemotherapy, she is doing well with a follow-up period of one and half years.
CONCLUSION
CPC in adults is a rare entity and presents with difficulty in diagnosis. The role of surgery and radiotherapy in the management of these cases is clear; role of chemotherapy needs to be defined in prospective studies.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES

| Fig. 1 CT brain showing space occupying lesion in the right frontal lobe
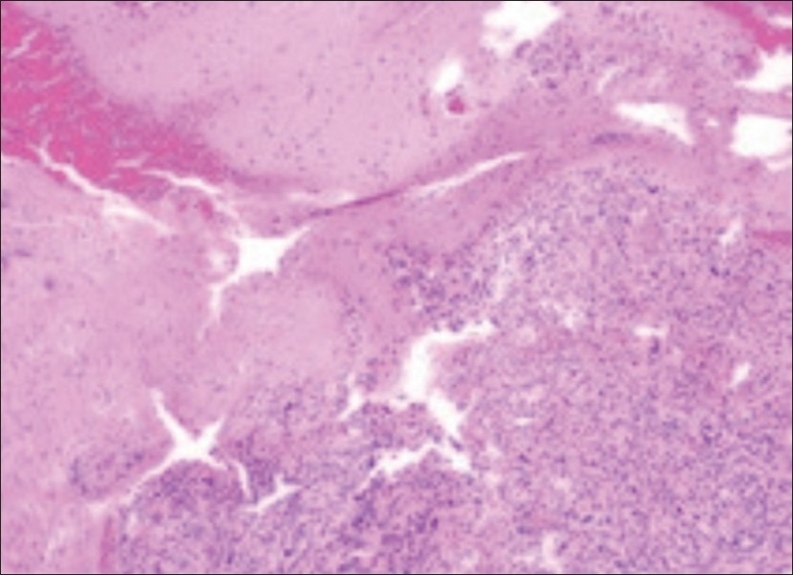
| Fig. 2 Solid sheet of choroid plexus carcinoma invading adjacent brain parenchyma (hematoxylin and eosin, original magnification ×100)
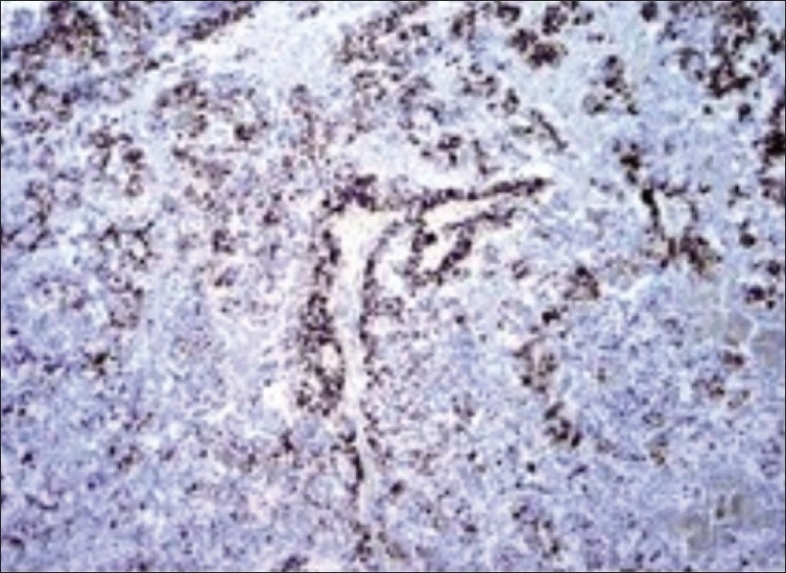
| Fig. 3 Positive glial fibrillary acidic protein staining in choroid plexus carcinoma (original magnification ×100)


 PDF
PDF  Views
Views  Share
Share

