A Case of Alveolar Rhabdomyosarcoma with Multifocal Pyomyositis Following Chemotherapy
CC BY-NC-ND 4.0 ? Indian J Med Paediatr Oncol 2018; 39(01): 93-95
DOI: DOI: 10.4103/ijmpo.ijmpo_138_16
Abstract
Pyomyositis is extremely rare after chemotherapy for nonhematological malignancies. We report a patient of alveolar rhabdomyosarcoma, who developed multifocal pyomyositis in bilateral lower limbs after the first cycle of neoadjuvant chemotherapy with vincristine, ifosfamide, mesna, and etoposide. The diagnosis of pyomyositis was reached after ultrasound and contrast-enhanced computed tomography scan of bilateral lower limbs. Staphylococcus and Streptococcus were isolated from pus. This patient was treated with 4 weeks of antibiotics, besides ultrasound-guided pus aspiration and open surgical debridement. To the best of our knowledge, no case of rhabdomyosarcoma with pyomyositis following chemotherapy has been reported so far.
Keywords
Chemotherapy - multifocal pyomyositis - rhabdomyosarcoma
Publication History
23 June 2021
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Pyomyositis is extremely rare after chemotherapy for nonhematological malignancies. We report a patient of alveolar rhabdomyosarcoma, who developed multifocal pyomyositis in bilateral lower limbs after the first cycle of neoadjuvant chemotherapy with vincristine, ifosfamide, mesna, and etoposide. The diagnosis of pyomyositis was reached after ultrasound and contrast-enhanced computed tomography scan of bilateral lower limbs. Staphylococcus and Streptococcus were isolated from pus. This patient was treated with 4 weeks of antibiotics, besides ultrasound-guided pus aspiration and open surgical debridement. To the best of our knowledge, no case of rhabdomyosarcoma with pyomyositis following chemotherapy has been reported so far.
Keywords
Chemotherapy - multifocal pyomyositis - rhabdomyosarcoma
Introduction
Pyomyositis, purulent infection of skeletal muscle, is a rare infectious disease. It is more common in tropical regions. It has a subacute course. Its pathogenesis is not well elucidated. Immunosuppression due to diabetes mellitus, HIV infection, prolonged use of corticosteroids, hematological malignancies, chemotherapy, chronic renal failure, or cirrhosis may be predisposing conditions. Pyomyositis as a complication of chemotherapy for nonhematological malignancies is extremely rare.
Case Report
A 27-year-old male, tobacco chewer, not a known case of any chronic illness, presented in January 2016 with left-sided upper neck swelling for 2 months. His performance status on Eastern Cooperative Oncology Group scale was 1. Examination revealed a conglomerate nodal mass in the left side of neck extending from level 2 to 4. Fine-needle aspiration cytology suggested metastatic poorly differentiated neoplasm. Contrast-enhanced computed tomography (CECT) scan of the neck and thorax revealed multiple left-sided neck nodes in all stations, largest measuring 6.2 cm ? 4.2 cm at Level II. Positron emission tomography-CT scan showed conglomerate left cervical lymph nodes and left supraclavicular lymph nodes. Biopsy from cervical lymph node revealed alveolar rhabdomyosarcoma with rhabdomyoblastic differentiation. On immunohistochemistry, the tumor cells were diffusely positive for CD56, desmin, and myogenin while negative for AE1/AE3, p63, synaptophysin, Melan-A, HMB-45, chromogranin, and leukocyte common antigen. He was planned for neoadjuvant chemotherapy followed by locoregional therapy. He received the first cycle of chemotherapy with vincristine, etoposide, and ifosfamide with mesna (VIME). Injection Vincristine was repeated one week later. He presented on day 23 after first cycle of VIME with pain in the right leg for 3 days and swelling on the posterior aspect of the left thigh for 2 days. There was no history of trauma. Examination revealed swelling and tenderness in the right calf, feeble pulsation in the right dorsalis pedis artery, and two distinct nontender soft lumps, 3 cm ? 2 cm each, located posteriorly on upper one-third of the left thigh. He was hemodynamically stable and had fever 102 F. Ultrasound of lower limbs revealed bulky right gastrocnemius muscle appearing darkly hypoechoic and showing posterior acoustic enhancement suggestive of myositis with early changes of necrosis. Neither liquefied collection nor any evidence of deep vein thrombosis was seen. Targeted ultrasound at the sites of swelling in the left thigh revealed collection with moving internal echoes in the subcutaneous plane and surrounding hyperechoic fat suggestive of inflammation without the involvement of the underlying muscles. Blood investigations revealed a total leukocyte count of 41,000/?L, Grade 1 transaminitis, and normal renal functions. CECT scan of bilateral lower limbs revealed multiple peripherally enhancing abscesses in the muscle plane in both lower limbs involving the right vastus medialis, left adductor magnus, right gastrocnemius, and left tibialis posterior [Figure 1] and [Figure 2]. He was hospitalized and started on intravenous antibiotics after drawing blood for culture. During hospital stay, he was treated with antibiotics ? cefepime-tazobactam, meropenem, amikacin, teicoplanin and clindamycin. He responded to antibiotics. Serial ultrasound examinations showed the formation of abscess. Pus was aspirated twice under ultrasonographic guidance from the left thigh, right gastrocnemius, and right vastus medialis. Open surgical debridement of pus from the right gastrocnemius and right vastus medialis was performed after 10 days of hospital stay [Figure 3]. Pus culture showed Streptococcus species on one occasion, sensitive to amikacin, cephalexin, and azithromycin; on another occasion, pus culture showed Staphylococcus sensitive to amikacin, ofloxacin, and cephalexin. Blood culture was sterile. He was discharged after 2 weeks of hospitalization. After discharge, he was started on oral metronomic chemotherapy with cyclophosphamide and etoposide for 2 weeks. After the conclusion of metronomic chemotherapy, he was planned for three cycles of vincristine, cyclophosphamide, and dactinomycin as neoadjuvant chemotherapy followed by locoregional therapy and adjuvant chemotherapy. He has completed his neoadjuvant chemotherapy with good tolerance. The neck masses have completely resolved.{Figure 1}{Figure 2}{Figure 3}
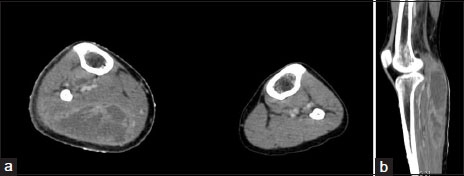
|?Figure.1Axial (a) and sagittal (b) reformats of the patient with peripherally enhancing abscess in the right gastrocnemius muscle
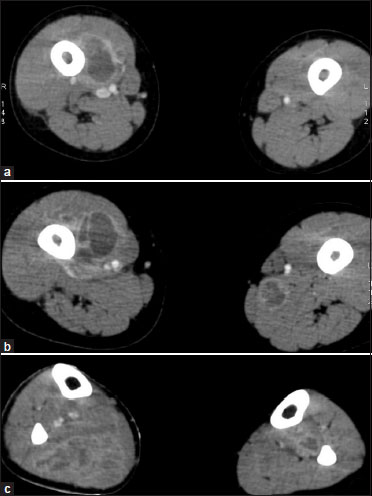
|?Figure.2Same patient with similar peripherally enhancing abscesses in the right vastus medialis (a), the left tibialis posterior muscle (b), and small abscess in the left adductor magnus muscle (c)
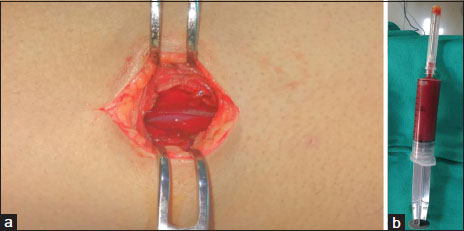
|?Figure.2Intraoperative picture of the opened cavity (a) in the right gastrocnemius muscle showing a cavity with white thick shaggy walls. About 30 ml of hemorrhagic tinged pus was aspirated (b)
Discussion
Pyomyositis, as a complication of chemotherapy, has been rarely reported. It has been reported in patients of acute lymphoblastic leukemia,[1] acute myeloid leukemia,[2] myelodysplastic syndrome,[3] multiple myeloma, endometrial cancer,[4] lung cancer,[5] breast cancer,[6],[7] retroperitoneal teratoma,[8] colon cancer,[7] and glottic cancer.[7] Anthracyclines,[6] vinca alkaloids,[1] corticosteroids,[1] and taxanes [4] have been implicated in previous reports. The initial symptoms of myalgias can be confused with vincristine-induced pain. In the early stage of pyomyositis, examination does not reveal any specific findings. Signs such as fever, chills, and erythema are uncommon. Hence, early diagnosis of pyomyositis is difficult. Due to the delay in diagnosis, complications such as compartment syndrome, arthritis of adjacent joints, multiple muscle abscesses, and sepsis may occur. This patient received vincristine and presented with multiple muscle abscesses in both lower limbs. In early stages, ultrasonography reveals only altered echogenicity, which is nonspecific. In the late stage of suppuration, fluid collection may be seen. Staphylococcus aureus is the most common pathogen, followed by Streptococcus.[9] Other organisms isolated include Bacteroides fragilis, Stenotrophomonas maltophilia,[3] pneumococci, Haemophilus influenzae, Gram-negative enteric bacilli, and anaerobes. In this patient, Staphylococcus and Streptococcus were isolated in pus culture. Blood cultures are positive in 5%?10% patients only. This patient had no growth in blood culture. Some patients are cured with antibiotics alone,[10] whereas others require drainage of pus. This patient was treated with antibiotics for total 4 weeks, ultrasound-guided aspiration of pus, and open surgical debridement. This report highlights an unusual focus of infection ? multifocal pyomyositis after chemotherapy for rhabdomyosarcoma. When a patient on chemotherapy presents with limb swelling and tenderness, pyomyositis should also be considered in the differential diagnosis apart from cellulitis, deep vein thrombosis, and osteomyelitis.
Conflict of Interest
There are no conflicts of interest.
References
- ao KL, Hung GY, Hwang B.?Pyomyositis during induction chemotherapy for acute lymphoblastic leukemia. J Chin Med Assoc 2006; 69: 184-8
- ukushima T, Iwao H, Nakazima A, Miki M, Sakai T, Sawaki T.?et al.?MRSA-pyomyositis in a patient with acute myelogenous leukemia after intensive chemotherapy. Anticancer Res 2009; 29: 3361-4
- sai SH, Chao TY, Chou TD, Dai MS.?Stenotrophomonas maltophilia septicemia with pyomyositis in a chemotherapy-treated patient. Ann Hematol 2003; 82: 452-4
- ingh P, Chan W, Blomfield P, McIntosh R.?Pyomyositis after chemotherapy for endometrial cancer. Int J Gynecol Cancer 2010; 20: 1256-8
- amada K, Wasa J, Sugiura H, Horio Y.?A case of multiple pyomyositis after chemotherapy for lung cancer. Gan To Kagaku Ryoho 2006; 33: 837-40
- eith BD, Bramwell VH.?Pyomyositis after chemotherapy for breast cancer. Am J Clin Oncol 2000; 23: 42-4
- hiu SK, Lin JC, Wang NC, Peng MY, Chang FY.?Impact of underlying diseases on the clinical characteristics and outcome of primary pyomyositis. J Microbiol Immunol Infect 2008; 41: 286-93
- aguire J, Kaye SB.?et al.?Psoas abscess: Unusual complication of effective chemotherapy for teratoma. Br Med J (Clin Res Ed) 1985; 290: 1870
- hiedozi LC. Pyomyositis?Review of 205 cases in 112 patients. Am J Surg 1979; 137: 255-9
- Gubbay AJ, Isaacs D.?Pyomyositis in children. Pediatr Infect Dis J 2000; 19: 1009-12
Address for correspondence
Publication History
23 June 2021
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
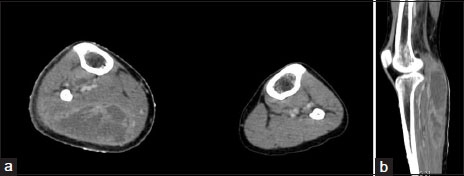
|?Figure.1Axial (a) and sagittal (b) reformats of the patient with peripherally enhancing abscess in the right gastrocnemius muscle
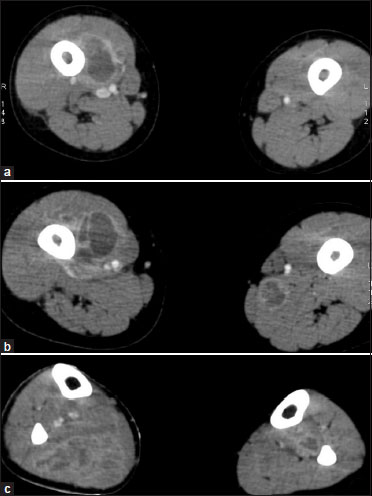
|?Figure.2Same patient with similar peripherally enhancing abscesses in the right vastus medialis (a), the left tibialis posterior muscle (b), and small abscess in the left adductor magnus muscle (c)
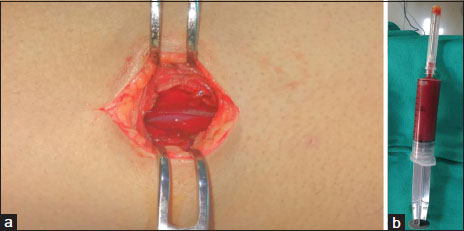
|?Figure.2Intraoperative picture of the opened cavity (a) in the right gastrocnemius muscle showing a cavity with white thick shaggy walls. About 30 ml of hemorrhagic tinged pus was aspirated (b)
References
- ao KL, Hung GY, Hwang B.?Pyomyositis during induction chemotherapy for acute lymphoblastic leukemia. J Chin Med Assoc 2006; 69: 184-8
- ukushima T, Iwao H, Nakazima A, Miki M, Sakai T, Sawaki T.?et al.?MRSA-pyomyositis in a patient with acute myelogenous leukemia after intensive chemotherapy. Anticancer Res 2009; 29: 3361-4
- sai SH, Chao TY, Chou TD, Dai MS.?Stenotrophomonas maltophilia septicemia with pyomyositis in a chemotherapy-treated patient. Ann Hematol 2003; 82: 452-4
- ingh P, Chan W, Blomfield P, McIntosh R.?Pyomyositis after chemotherapy for endometrial cancer. Int J Gynecol Cancer 2010; 20: 1256-8
- amada K, Wasa J, Sugiura H, Horio Y.?A case of multiple pyomyositis after chemotherapy for lung cancer. Gan To Kagaku Ryoho 2006; 33: 837-40
- eith BD, Bramwell VH.?Pyomyositis after chemotherapy for breast cancer. Am J Clin Oncol 2000; 23: 42-4
- hiu SK, Lin JC, Wang NC, Peng MY, Chang FY.?Impact of underlying diseases on the clinical characteristics and outcome of primary pyomyositis. J Microbiol Immunol Infect 2008; 41: 286-93
- aguire J, Kaye SB.?et al.?Psoas abscess: Unusual complication of effective chemotherapy for teratoma. Br Med J (Clin Res Ed) 1985; 290: 1870
- hiedozi LC. Pyomyositis?Review of 205 cases in 112 patients. Am J Surg 1979; 137: 255-9
- Gubbay AJ, Isaacs D.?Pyomyositis in children. Pediatr Infect Dis J 2000; 19: 1009-12


 PDF
PDF  Views
Views  Share
Share

